As a healthcare provider do you want to know – How to Use Remote Patient Monitoring and Get CMS Reimbursement?
Remote Patient Monitoring (RPM) has leaped into the spotlight since the COVID-19 pandemic. Though versions of RPM have been around since the 1970s, the Centers for Medicare and Medicaid Services (CMS) didn’t fully reimburse providers for these critically needed services until 2019.
In January 2020, CMS created more billing codes that allow healthcare providers to extend the use of remote patient monitoring (RPM) for more situations.
If you are a provider who believes RPM would be best for your patients, there are several guidelines you need to follow to ensure complete compliance with CMS guidelines.
To take full advantage of the RPM benefits and reduce risk, providers need to follow CMS guidelines. This is especially true when they apply for reimbursement. Here’s a quick guide to help your practice implement RPM for your Medicare and Medicaid patients.
Choose the Right RPM Tools
First, consider your patients’ needs. Often, seniors receiving Medicare coverage won’t have the technological savvy to learn how to use current technology. If you can make the monitoring process easy to implement, the more likely patients will keep up with their prescribed regimen that you have provided
Simplify to ensure compliance
Many RPM technology companies provide only devices that need a smartphone app to work. However, many seniors may lack a smartphone or not be familiar with all of the phone functions they may need for RPM.
When they become frustrated, they stop monitoring their condition. Non-compliance, in turn, gives rise to hospital readmissions.
For healthcare providers, you need to know, you won’t receive reimbursement if the patients don’t monitor. If you’re affiliated with a hospital, CMS might penalize your hospital if readmissions rise above a specific number.Why take those risks? Healthcare providers can choose an app-free RPM system. You will find that it can be a game-changer when it comes to compliance.
Delegate administration tasks to streamline your workflow
Since your main focus is patient care, choose an RPM company that takes care of the administrative tasks for you. Your practice can save money (and time) when you outsource administrative tasks such as:
- Obtaining your patients’ consent
- Creating patient records
- Onboarding your patients and staff
- Shipping monitoring devices to your patients
- Reviewing patient data to ensure compliance with CMS’s billing requirements
Get Your RPM Program Up and Running
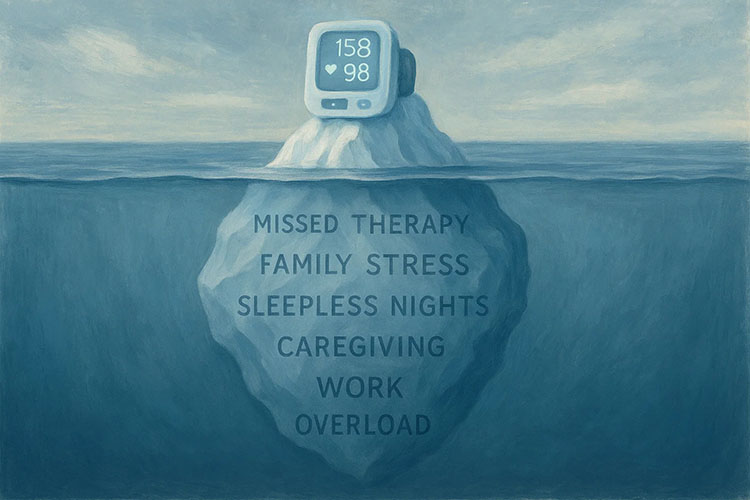
Once you’ve chosen your RPM company , you can identify which of your patients could benefit from remote monitoring. Patients with chronic conditions where daily monitoring would provide valuable patient data are good candidates for RPM. , Chronic condition patients include those with diabetes, hypertension, COPD, and certain cardiac issues, benefit from daily monitoring.
Check your state regulations and insurance provider to see if you need an upgrade in your malpractice coverage for RPM. Make sure that all staff are on board with their roles and that your RPM services company has adequate support in place should technical issues occur.
Here’s a rundown of how to use RPM once you have the correct company in place:
- Prescribe RPM for patients who could benefit from daily monitoring. Since most in-person visits for chronic conditions involve taking physiologic measurements, remote monitoring and intervention can help reduce time-consuming in-office routine care. Patients who have difficulty coming to the office because of distance or risk of contracting communicable diseases are all excellent candidates.
- Set up your patients for monitoring: If you do not delegate your RPM company to obtain it, you will need to obtain your patients’ consent. Unless delegated, you will need to teach patients how to operate their monitoring devices, and provide them with their monitoring devices, either in person or through shipping.
- Schedule regular monitoring check-ins: Industry standards are to communicate with your patients through a video call or phone conversation biweekly to monthly. Let your patients know when they need to take their measurements. Make sure they know how to get help in case they have difficulties with the process.
- Keep an eye on your patients’ data: Most RPM systems, including Medek, send data to a HIPAA-compliant portal. You’ll have a dashboard on which you can look at your patients’ current results, history, trends, and review their care plan, in case the data indicates that you should make a change.
A Medek RPM system provides you with results in real-time, allowing you to make medication and other changes quickly. In addition, our medical staff reviews your patients’ data, freeing your staff to spend more time with patients with more pressing issues.
Comply with CMS Rules to Ensure Reimbursement
To receive reimbursement, you must adhere to the specifications CMS outlines for each service rendered. The AMA'S (American Medical Assoc) CPT® codes define the parameters you need to cover to meet their requirements to obtain reimbursements.
Figure 1:
| CPT® Code | Service Description | Notes |
| 99453 | Sets the parameters for RPM measurements, including weight, blood pressure, pulse oximetry, respiratory flow rate, and other routine measurements. It also covers the hardware (medical device), software (HIPAA compliant portal) setup process and patient education on how to conduct each measurement. | There is no work relative value unit (wRVU) assigned, nor is there any requirement for practitioner work to bill for these services. |
| 99454 | Provides guidelines for supplying the monitoring device, daily recordings, with a focus on the devices used, as well as on guidelines involving daily recordings or programmed alerts every 20 days. | There is no work relative value unit (wRVU) assigned, nor is there any requirement for practitioner work to bill for these services. The device that you use to measure and transmit your patient’s physiologic data or create alerts if issues arise must be in good working condition and be able to process the data without error. |
| 99457 | Sets parameters for the initial 20 minutes of RPM treatment services that arise from physiologic monitoring results during one calendar month. Treatment services must be rendered by a physician, clinical staff member, or other qualified healthcare provider. These services require interactive communication with the patient, or their caregiver. | The supervising physician or practitioner does not need to be the same person administering the patient’s treatment in general. You do, however, need to bill this code using the National Provider Identifier (NPI) of the supervising physician or practitioner. |
| 99458 | If the treatment services arising from physiologic monitoring results require an additional 20 minutes, CMS specifies that practitioners use this code for each 20-minute period. | The supervising physician or practitioner does not need to be the same person administering the patient’s treatment in general. You do, however, need to bill this code using the National Provider Identifier (NPI) of the supervising physician or practitioner. |
Documentation that you met the criteria for each service is essential for receiving reimbursement. Additionally, you must meet the following general requirements:
- A face-to-face visit: Patients who have not had a face-to-face visit for a year, and new patients must have such an in-person visit before remote monitoring can begin.
- Patient consent: Providers must obtain consent from each patient before RPM begins. We strongly advise that providers document each patient’s consent.
- Physician’s or practitioner’s orders: Either a physician or a non-physician practitioner must order RPM. Again, you must document the provider’s order in the patient’s records.
Administrative services that you can outsource to your RPM company , then the more time you can spend with patients with critical needs. Accurate, error-free, well-documented measurements and records are essential for receiving reimbursement from CMS. Medek RPM provides healthcare practices with a full-service RPM platform designed to improve patients’ health through accurate measurement, real-time reporting, and a robust, intuitive interface. It increases billing revenues with thorough video and voice calls that reviews the patient’s data with the patient. This ensures you have meet the CMS’s requirements. With an automated system that sends your billers all you need to get your reimbursement, Medek RPM helps you to keep helping others. To request a full product demo, get in touch with the Medek team today.