The pandemic proved how essential telehealth services and Remote Patient Monitoring (RPM) can be, and the ways Centers for Medicare and Medicaid (CMS) suggest utilizing them. In November 2021, the agency announced changes to its fee schedule to provide reimbursement for physicians who provide these services.
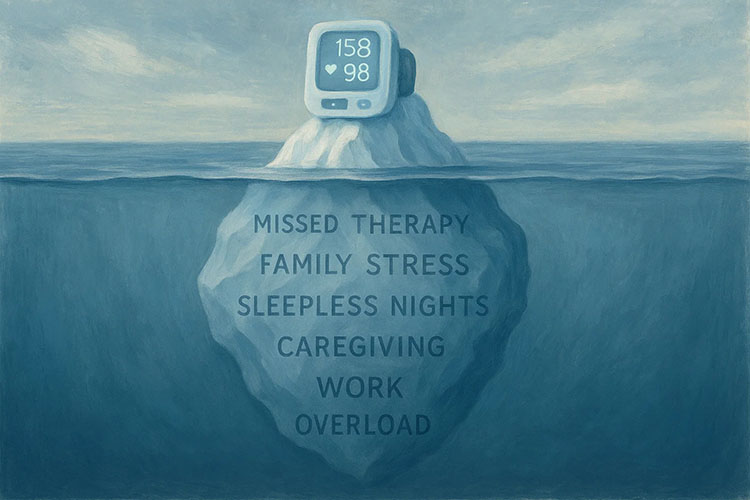
With RPM, CMS recognized that physicians are bringing care directly into their patients’ homes. This service offers a significant benefit for those who need chronic care management.
For 2023, the CMS Fee Schedule includes changes to make RPM even more practical for practices. It starts with an expansion of remote therapeutic monitoring codes to broaden the use of reimbursement for RPM.
What is Remote Therapeutic Monitoring?
CMS defines remote therapeutic monitoring as data that is non-physiological. This would be monitoring that extends beyond basic vital signs and blood sugar. It would include the general state of the patient’s health and how they respond to medications.
With this change, CMS recognizes that the RPM service needs to cover things that are not necessarily quantifiable with data. Practices can get reimbursement for general medicine that goes beyond the numbers. The expansion of the codes for RPM will now include four new HCPCS G-Codes designed to improve a patient’s access to RPM and open up “incident to” billing for the practice.
New Remote Codes for Behavioral Health and Chronic Pain Management
CMS is also adding codes for Behavioral Health and Chronic Pain Management. Behavioral Health reimbursement codes will include psychotherapy for crisis care. For Chronic Pain Management, the new HCPCS code is for RPM of pain intensity. This means clinicians can use remote technology to monitor patient pain and management plans.
What About Remote Patient Monitoring Codes?
While these new codes do not cover all RPM services, some changes are worth noting. One example is, CMS is extending the RPM limitations in a Public Health Emergency (PHE). The proposed rule will extend PHE allowances to 151 days past the end of the crisis.
They also implemented the Consolidated Appropriations Act of 2022, allowing audio-only telehealth services in underserved areas. This will also extend to physical therapists, speech pathologists, and audiologists.
A Breakdown of Additional CMS Code Changes for Telehealth and RPM
Consider some of the proposed changes for 2023 that affect telehealth and remote patient monitoring services.
Three New Codes for Evaluation and Management Telehealth Services
- GXXX1 for Prolonged hospital inpatient or observation care evaluation and management that goes beyond the primary service time. The code adds 15 minutes with or without direct patient contact.
- GXXX2 for Prolonged nursing facility evaluation and management services that goes beyond the primary service time. The code adds 15 minutes with or without direct patient contact.
- GXXX3 for prolonged home or residence evaluation and management beyond the primary service time. The code adds 15 minutes with or without direct patient contact.
Discontinue Separate Reimbursement of Telephone Evaluation and Management Services
CMS indefinitely denied requests to add these services to the Medicare Telehealth Services List. CMS stated that “except for certain telemental health services, two-way interactive audio-video telecommunications technology would remain the Medicare requirement for telehealth services after the PHE. This is because Section 1834(m)(2)(A) of the Social Security Act requires telehealth services to be analogous to in-person care by being able to replace the face-to-face encounter.”
In other words, telephone-only services will not have separate reimbursement 151 days after a public health emergency expires. Instead, they will revert to the bundled status.
Fifty-four New Codes for Telehealth Services
CMS is also proposing the addition of 54 new telehealth codes that will expire at the end of 2023, unless renewed. These codes cover services in nine separate categories:
- Therapy
- Electronic analysis of implanted neurostimulator pulse generator/transmitter
- Adaptive behavior treatment and assessment
- Behavioral Health
- Ophthalmologic
- Cognition
- Ventilator management
- Speech therapy
- Audiologic
These are category three codes. All category three codes are scheduled to expire at the end of 2023.
Though some of these changes are temporary, the CMS is showing that telehealth and Remote Patient Monitoring will continue to be part of our healthcare industry. Private practices will need to stay informed of changes to maximize quality healthcare and positive cash flow for their practices.
Medek RPM is one of the fastest growing RPM companies in the US. Begin a conversation with a Medek Representative today.