In 2020, the definition of “health literacy” was updated and adopted by the Centers for Disease Control and Prevention (CDC). They distinguished organizational health literacy from personal health literacy, which they described as, “…the degree to which individuals have the ability to find, understand, and use information and services to inform health-related decisions and actions for themselves and others.”1
This new definition highlights two important factors around personal health literacy:
- Emphasizes patients’ abilities to actually use health information, rather than just understand it.
- Focuses on the ability to make informed decisions.2
The Medek Clinical Care team is here to describe how Remote Patient Monitoring (RPM) can be an extremely effective strategy that assists patients in achieving both of the above critical CDC factors. RPM offers several other benefits to your patients and to your medical practice that can greatly contribute to better patient outcomes, higher patient satisfaction, cost-effective care, and expansion in revenue opportunities.
How Does Remote Patient Monitoring Work?
Remote patient monitoring (RPM) is also called remote physiologic monitoring, and sometimes remote therapeutic monitoring. The Medek RPM system includes the following devices: weight scale, pulse oximeter, blood-glucose meter, and blood pressure cuff. When patients take their measurements, data is incorporated into their medical record. All processes are HIPAA-secured cellular connections.
You and your clinical team can review patient data 24 hours per day. The Medek Care Team also assesses patient status and immediately notifies your providers of any concerning trends or measures that might be considered outside the norm.
ADDITIONAL RESOURCE: Specifics on Medek’s available devices.
How Does RPM Improve Health Literacy?
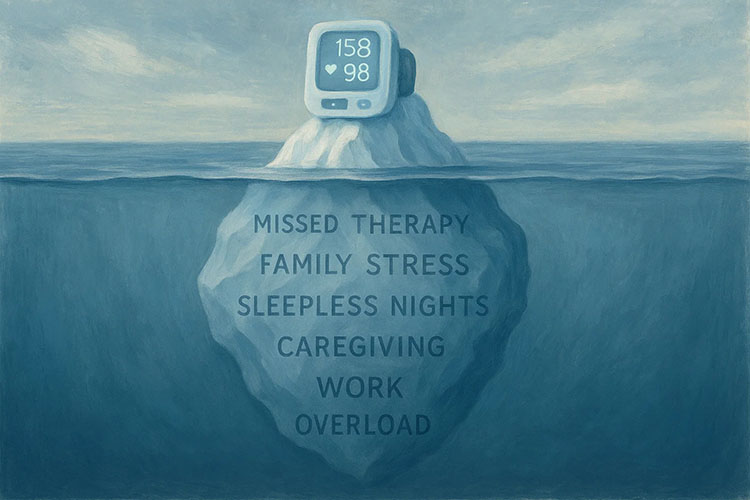
Each time a patient is tasked with taking their vital signs (e.g., heart rate, oxygen saturation, blood pressure, blood-glucose levels), they improve their health literacy abilities in the following ways, including (but certainly not limited to):
- Increasing self-confidence in using digital health devices.
- Understanding the importance of taking medications as prescribed.
- Learning which metrics may be considered ‘normal’ for their specific condition.
- Developing a sense of achievement as they manage their own health.
These skills empower patients to take a more active role in their health by changing personal lifestyle habits and living conditions.3 One of the major benefits of RPM is that it increases the capacity of patients to use their health information more effectively.
Medicare Reimbursement Policies
The Centers for Medicare and Medicaid Services (CMS) refers to RPM specifically as remote physiologic monitoring. They fully recognize its benefits as an intervention for chronic health conditions such as diabetes, asthma, and hypertension. CMS designated several applicable Billing codes:4,5
- 99453 – Initial set-up and patient education.
- 99454 – Data recording and programmed alerts.
- 99457 – 20 minutes per calendar month (cumulative) on patient care management.
- 99458 – Additional patient care.
ADDITIONAL RESOURCES:
- Using Remote Patient Monitoring to Increase Practice Revenue Without Bringing on New Patients
- A Deeper Dive into Medicare CMS Codes
Supporting Literature
When healthcare professionals help patients get started with RPM, the process in-and-of-itself is an excellent exercise in patient education. Patients gain additional understanding of disease processes, exacerbations, and when it may be appropriate to contact their physician’s office. 6
Particularly since the COVID-19 pandemic, researchers have been studying the value of RPM for patients and for clinicians. One scoping review on the use of pulse oximeters had a positive effect on patients’ sense of self-efficacy and motivation, both of which are important elements of health literacy. 7
A report from the National Committee on Quality Assurance (NCQA) strongly emphasizes the value of remote patient monitoring to improve health literacy. RPM can motivate patients to manage their own health as they learn to track trends in weight, blood pressure, and/or blood sugar levels. They gain a long-term understanding of their condition(s), which facilitates better-informed decisions about future care.8
Among the benefits are fewer unnecessary hospitalizations, lower healthcare costs, greater patient satisfaction, and a potential to expand services to hard-to-reach, rural areas.9
Beyond COVID-19
Although RPM was used prior to COVID-19, the many benefits of this connected technology were not completely realized. Remote physiologic monitoring became a lifesaver for patients who were older or had pre-existing conditions that made it problematic to go to the doctor’s office.
As the pandemic slowed down, the use of this innovative telehealth strategy has continued to grow. In fact, it is predicted that by 2024, approximately 30 million Americans will use remote patient monitoring.10
More Questions?
- Getting started with Medek Remote Patient Monitoring is easy. It requires no up-front costs for you or your patients. Our onboarding process is fast, and yet comprehensive. The Medek care team helps patients with the initial set-up and reaches out to them regularly. We have an excellent resource library so you can learn more about RPM anytime.
Give Us a Call at (866)336-3335 or Request a Demo
****
Sources
- Centers for Disease Control and Prevention [CDC] (Updated-2022, February 2). https://www.cdc.gov/healthliteracy/learn/index.html
- Ibid.
- World Health Organization. (n.d.) Improving health literacy. https://www.who.int/activities/improving-health-literacy
- Lacktman, N.M., Ferrante, T.B., Goodman, R.B. (2020, December 7) 2021 Medicare Remote Patient Monitoring FAQs: CMS Issues Final Rule. Foley and Lardner, LLP. https://www.foley.com/en/insights/publications/2020/12/2021-remote-patient-monitoring-cms-final-rule.
- Centers for Medicare and Medicaid Services. (2020, December 1). Final Policy, Payment, and Quality Provisions Changes to the Medicare Physician Fee Schedule for Calendar Year 2021. https://www.cms.gov/newsroom/fact-sheets/final-policy-payment-and-quality-provisions-changes-medicare-physician-fee-schedule-calendar-year-1
- Tripathi, S. (2017, September) GeoICT for meeting the needs of remote patient monitoring and healthcare. International Journal of Geoinformatics, 13(3). 1-10. 1074-Article%20Text-1113-1-10-20170924%20(1).pdf
- Rosic, T., Petrina, N., Baysari, M., Ritchie, A., & Poon, S. K. (2022). Patient and clinician use characteristics and perceptions of pulse oximeter use: A scoping review. International journal of medical informatics, 162, 104735. Advance online publication. https://doi.org/10.1016/j.ijmedinf.2022.104735
- Guzman, V. (2021, October 21). https://www.ncqa.org/digital-measures/resources/blogs/de22efbe-094f-41e9-bbc3-910e6678ae5e/#:~:text=LOGIN%20%26%20GET%20ACCESS%20Health%20care%20organizations%20should,and%20communication%2C%20understanding%20a%20patient%E2%80%99s%20beliefs%20is%20essential.
- Telehealth, Health and Human Services (HHS).gov. (2022, August 26). Telehealth and remote patient monitoring. https://telehealth.hhs.gov/providers/preparing-patients-for-telehealth/telehealth-and-remote-patient-monitoring/
- Dolan, S. (2022, January 11). The technology, devices, and benefits of remote patient monitoring in the healthcare industry. Insider Intelligence. https://www.insiderintelligence.com/insights/remote-patient-monitoring-industry-explained/
Additional Sources: Medek Website