The landscape of healthcare is witnessing profound changes, with Remote Patient Monitoring (RPM) emerging as a cornerstone. If you're seeking to understand this revolutionary shift or enhance your knowledge, our detailed guide to the five "W"s of RPM is tailored for you.
1. What is RPM?
RPM, at its core, is the digital bridge between patients and healthcare professionals. It involves patients, especially those grappling with chronic ailments, using FDA-approved medical devices1 within the comfort of their homes. These gadgets seamlessly transmit vital health readings to their healthcare providers through a secure, encrypted cloud. This real-time data exchange allows for timely interventions and personalized care.
2. Who stands to gain from RPM?
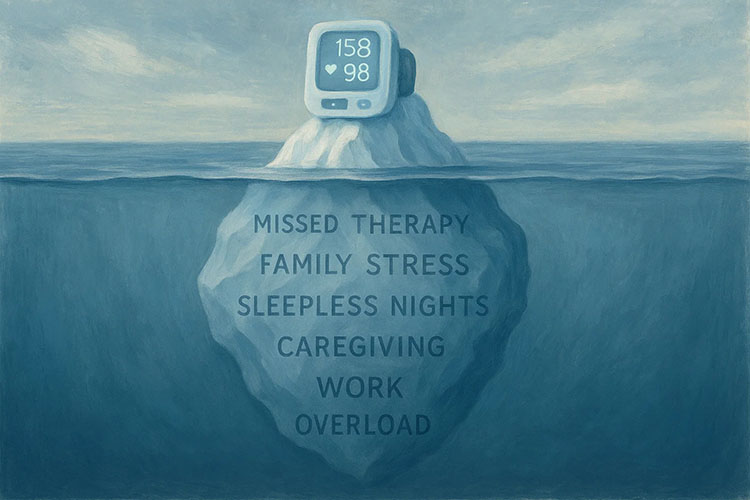
RPM in Practice: Consider John Smith, a hypertension patient. Equipped with an at-home BP Cuff (typically covered by insurance), he diligently sends daily readings after initial guidance. This data funnels directly to his medical team, which then actively monitors for any anomalies, ensuring that John receives immediate feedback and care recommendations. Essentially, patients battling a myriad of conditions, from diabetes and asthma to heart failure and beyond, can benefit from RPM. Each ailment has specific FDA-approved devices crafted to cater to their monitoring needs.
3. Why the paradigm shift to RPM?
America is home to over 133 million chronic health condition patients2. The conventional healthcare model often proved inefficient, with patients either inundated with frequent office visits or left to their own devices to record health statistics. This led to missed anomalies, inaccuracies, and disjointed care. RPM, with its real-time data relay, is the panacea, transforming patient-doctor communication into a streamlined, effective process.
4. Where does RPM come into play?
While RPM predominantly unfolds within the familiar confines of a patient's residence, it's far from static. Here are the benefits:
- No "white coat" anxiety3: Patients can record data without the stress of a clinical setting.
- Cost-effectiveness: Transport-related costs become redundant.
- Enhanced Adherence: The ease of RPM fosters better compliance with medical directives.
Further underscoring its flexibility, RPM devices are not confined to the home. Their portability ensures that patients can take them on vacations, to work, or any other locale. Comprehensive onboarding support, periodic check-ins, and monthly reviews are built-in features, assuring continuous patient engagement and understanding.
5. When is RPM most relevant?
For RPM to deliver its promise, regular health readings are pivotal. Predominantly, insurance plans, encompassing Medicare and Medicaid, stipulate readings for a minimum of 16 days monthly. Given life's unpredictability, most doctors advise daily recordings. This rhythm is punctuated by monthly professional consultations, annual physical visits, and spontaneous interventions whenever the data flags potential health concerns.
Implications & Opportunities: RPM is not just a monitoring tool. It's a paradigm shift. It paves the way for enhanced health outcomes, informed medical decisions backed by data, and even a smoother reimbursement process from agencies like CMS4.
For a deeper dive into RPM's transformative potential, Medek RPM, a frontrunner in the RPM domain in the US, offers a treasure trove of insights.
Footnotes:
- https://www.fda.gov/medical-devices/covid-19-emergency-use-authorizations-medical-devices/remote-or-wearable-patient-monitoring-devices-euas
- https://www.aha.org/system/files/content/00-10/071204_H4L_FocusonWellness.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7318827/
- https://www.usa.gov/agencies/centers-for-medicare-and-medicaid-services