Remote Patient Monitoring (RPM) is a newer concept in the healthcare industry. There are plenty of myths regarding this technology. Despite the many benefits, some practices still fail to embrace this innovative option, and misconceptions are part of the reason why. Consider these myths regarding RPM and why they are not fact.
Myth 1: RPM Is Expensive
The idea of wearable devices and telehealth software probably does make adding this service sound costly. It doesn’t take as much startup capital as you might think. Creating a platform with just a couple of devices to start and a few data points to measure can provide a foundation to build from and give you an idea of the need.
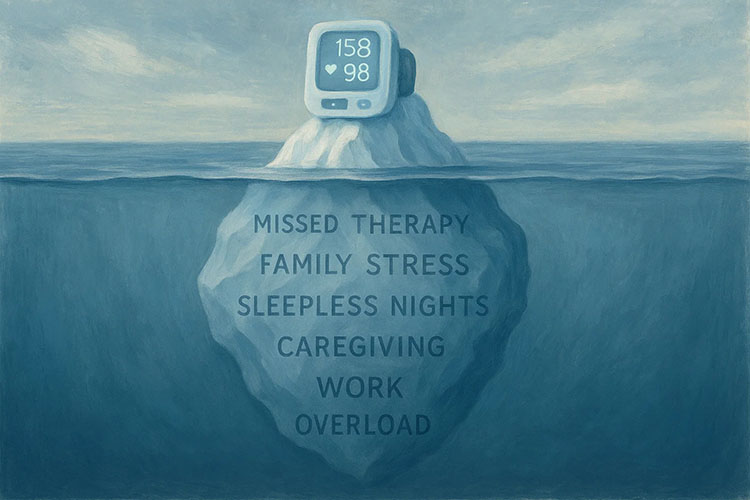
With even rudimentary data, clinicians can identify trends and determine how beneficial the service is to their community. RPM will also lower overhead costs for the practice because there should be fewer in-person office visits while improving patient outcomes. With Remote Patient Monitoring, physicians don’t have to rely on patient self-reporting to understand if a treatment is working or not. The improved efficiency opens up time for more patients and services.
Myth 2: RPM is Challenging to Implement
RPM is technology, so it can feel like it would be challenging to implement. Onboarding patients with new devices will take some time, too. There is a learning curve for staff, but support is usually available.
Also, you can screen the patients for digital literacy and use RPM initially on the ones most likely to understand its functioning. This will give the care team time to acclimate to the technology. The challenges will become less significant after a while.
Myth 3: RPM Is Not Secure
Patient data safety is always a concern in healthcare. However, RPM platforms have security measures in place to protect sensitive information. This technology must be compliant with the same security standards set by the Health Insurance Portability and Accountability Act (HIPAA) as any other platform, including patient portals and electronic records systems.
Myth 4: RPM is Too Automated and Takes the Human Element Out of Healthcare
RPM is not meant to replace direct communication and patient treatment; it simply supplements it. An effective doctor-patient relationship requires good communication, and RPM adds another layer. It also can be a tool for patient education. It is one thing to hear a care provider explain the benefits of certain behavioral changes and something else to see those changes occur first-hand. With RPM, patients become members of their own care team, enhancing their sense of importance, not reducing it.
Myth 5: RPM Does Not Provide Revenue
The Centers for Medicare and Medicaid fully embrace telehealth and Remote Patient Monitoring services. They recently implemented new billing codes for them, making reimbursable for some patients. Private insurance companies will follow suit eventually, making RPM a new revenue stream. The sooner practices start using it, the more revenue it will bring to their businesses.
Myth 6: Remote Patient Monitoring Only Works with High-Speed Internet
While it is true that most of these devices require Wi-Fi to function, there are other options. Bluetooth devices, for instance, would link to a cellular network. Also, the use of RPM and telehealth during the pandemic bubbled the need for better broadband in underserved areas to the surface. As a result, many communities are creating initiatives to improve their service options.
Myth 7: Remote Patient Monitoring and Telehealth are the Same Things
RPM is a form of telehealth but perhaps not what most people associate with the word. For most, telehealth is a virtual office visit. RPM is not that, although it can work in conjunction with it. RPM can be separate for telehealth office visits.
It uses devices to monitor conditions while a patient is at home. It allows the care team to analyze data and use it to follow the patient’s condition and determine the failure or success of treatments. RPM can also detect a problem before it becomes an emergency. Follow-ups can be virtual or in-person.
Myth 8: RPM has Limited Usage
RPM is about targeted care and long-term health and wellness. Remote monitoring can help address chronic health management for obesity, heart disease, or diabetes. It can also be beneficial for post-discharge rehabilitation. The fact is providers are only beginning to understand the benefits that come with remote patient management.
Find out more about RPM by contacting us today. Medek RPM offers a complete remote monitoring solution.